Your melatonin questions, answered!
When I talk to my patients about their mental health, we ALWAYS discuss sleep. It’s what I call a non-negotiable focus of mental health recovery. In my practice I’ve observed a pattern of dangerous self-treatment when it comes to trying to get more sleep. More often than not my patients are reaching for over the counter medications and supplements, in particular, melatonin. In this article, we’re going to cover the basics of melatonin and its safe supplementation. Skip to the end if you just want the ‘Need to Know. But I’d encourage you to read the article because knowledge is empowering to your health!
 Topics to be covered:
Topics to be covered:
- What is melatonin?
- Who should take melatonin?
- Melatonin supplementation in children & teens
- What is the best time to take melatonin?
- How much do I take?
- How much is too much?
- No all supplements are created equal!
- More reasons ‘less is more’
- I’ve heard melatonin treats cancer. Is this true?
- Summary
- Dr. Culver’s ‘Need to Know’
What is Melatonin?
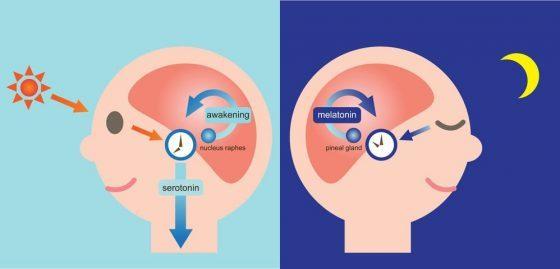
Melatonin is a HORMONE produced by the pineal gland, found just above the brain stem. It’s made from an amino-acid called Tryptophan. Remember when you learned that turkey makes you sleepy because it has high levels of tryptophan? Well, this is why! Tryptophan, through a series of enzymes, becomes melatonin.
The purpose of the pineal gland is to regulate our sleep-wake cycle, known as the circadian rhythm, and it does this by regulating the production of melatonin. The production and excretion of melatonin are triggered by variances in light levels. Low, or ‘Dim Light’, levels stimulate nerves that cause the release of norepinephrine at the pineal gland cells. When the sun sets, melatonin is triggered to be released. And contrary, blue (tablets/computers) and bright lights will have a melatonin production lowering effect, keeping your mind and body wide awake! Studies have theorized that norepinephrine stimulates the production of melatonin in three possible ways: either by 1) increasing the formation of a melatonin-forming enzyme, 2) increasing tryptophan transport into the pineal gland, or 3) inhibiting serotonin breakdown. The key thing to remember is that melatonin does not force sleep. Rather, it signals to the body that it is bedtime. This is why if you’ve had your sleep disrupted (jet lag), melatonin can reset your confused body and brain.
Who should take melatonin?
Everyone’s needs are different so talking with a doctor is the best thing to do. That being said, there are numerous studies reporting sleep initiation efficacy and anti-proliferation (anti-cancer) properties. It’s use in people with depression is surprising. One study showed that adding melatonin to someone who takes SSRIs (Prozac) does not positively (or negatively) impact the anti-depressive effects of these medications. Basically, if you’re on depression medication, melatonin will help with initiating sleep, but doesn’t improve depression symptoms. This does not mean that sleep won’t help depression, it just means melatonin won’t. Confusing yet?
What about melatonin supplementation in children and teens?
Several studies support melatonin use in children with sleep onset insomnia who may need long-term medication therapy, including those with autism spectrum disorder (ASD) or ADHD. It should not be used in healthy children without sleep problems to “promote restful sleep,” or in adolescents to force sleep onset and accommodate early school start times. Studies of melatonin for durations up to 4 years have failed to demonstrate adverse effects in children. However, it is important to know that long-term side effects can include suppression of sex hormones (the hypothalamic-gonadal axis). Rapid discontinuation in these circumstances could cause early puberty. I typically suggest my patients start by taking 0.3 mg a few hours before bed and to adopt sleep hygiene practices that will help to prevent the long-term use of melatonin.
When is the best time to take melatonin?
There are two answers to this question depending upon the symptoms you’re targeting. Normally, the brain begins to produce melatonin around 9pm. If you’re looking to encourage your body’s own production of melatonin, then taking melatonin 3 hours before your bedtime in a small dose is best because exogenous melatonin (supplementation) given earlier than the time of its usual endogenous (made by the brain) secretion helps to shift the circadian rhythm earlier.
Plasma levels of melatonin peak within one hour of administration. Therefore, if you want to fall asleep earlier to help re-establish a healthy bedtime (sleep onset insomnia), then taking melatonin 30 minutes to 1 hour before wanted sleep is recommended.
If you’re wide awake in the middle of the night, taking an additional dose will not help.
How much do I take?
The ideal dose of melatonin has not been standardized because it varies upon age and purpose.
For young adults, a dose of 0.1-0.3mg before sleep is adequate because it will raise nighttime plasma concentrations into the normal range. In my practice we stay low, at physiologic dosing, 0.5 – 1.5 mg. There are times when more is warranted, but remember, it should be used to establish bedtime habits, not as a sleeping pill.
How much is too much?
At high doses melatonin can be considered a hypnotic and won’t be more effective when you go over the recommended dose (< 3 mg). In 2005, MIT conducted a study which found that high doses of melatonin are effective for just a few days. But after that, the impact stops. Other research suggests that when melatonin receptors in the brain are exposed to too much of the hormone, the receptors become unresponsive. Meaning, melatonin will stop doing what it’s supposed to do. Other studies have found that doses above 1mg can leave people feeling drowsy in the morning. Although melatonin is considered generally safe and non-toxic, it is worth noting that some dosages, such as 10mg, can raise plasma concentrations to 60 times their normal values!
Not all supplements are created equal
As with all supplements and vitamins, melatonin is not regulated by the FDA. Because of this, available formulations will vary in accuracy of concentration. Erland reports a review of 31 commercially available melatonin supplements found that actual content varied from -83% – +478% and lot to lot variability was as much as 465%. Additionally, 26% of the samples contained serotonin as a contaminant. My recommendation is to purchase physician-only brands. They’re likely to be higher quality and have higher testing standards than those that aren’t.
More reasons that less is more!
Melatonin can affect fertility! In women, it can change progesterone, estradiol, luteinizing hormone and thyroid levels. In men, regular use of the “darkness hormone” can lower libido and can affect sperm – both decrease the count and slow it down. Remember, high levels of melatonin can suppress puberty in children. Additionally, too much melatonin taken at once can cause headaches, dizziness, nausea, or irritability. Very high levels of melatonin are associated with daytime grogginess, tiredness, and hypothermia.
I’ve heard melatonin treats cancer. Is this true?
Cure, treat, prevent entirely? No. There is no supportive evidence that is definitive.
Support existing therapies? YES!
The ideal dose for the supportive tumor suppression is not standardized and the type of cancer that it is best for is not agreed upon (though there are numerous studies related to hormonal cancers). For example, treatment in the prevention and presence of fibrocystic breasts, ovarian cysts, myomas, uterine fibromas, or endometrial thickening, 15–20 mg can be administered depending on the intensity of the disease.
Several clinical studies have shown that total daily doses of 20-40mg, up to 1000 mg of melatonin administered via slow IV, are tolerated and considered useful and beneficial in cancer patients. Patients diagnosed at an initial/early stage of disease can be given 30mg of melatonin orally. Di Bella reports numerous clinical studies have shown that patients with advanced or terminal stages of cancer, who no longer respond to traditional treatments, can benefit from high doses of melatonin. These patients could consider taking upwards of 100mg melatonin daily.
BUT! It goes without saying (I hope!), please DO NOT use melatonin if you have cancer or for cancer prevention before discussing it with a doctor who is familiar in its adjunctive use. It’s a hormone. It’s a powerful tool. It should be respected. The OncANP can be a resource for patients looking for naturopathic doctors who have post-doctoral training in oncology and who would be familiar with melatonin and its use in cancer.
The End. Asleep yet?
In summary, melatonin is considered to be safe, and in little doses, it is. It will help in re-establishing healthy sleep patterns (ie. Jet Lag) but not with sleep disorders such as insomnia. If you have sleep difficulties, it’s best to consult your doctor. There may be other underlying problems or non-supplemental and non-pharmaceutical options available to you.
Dr. Culver’s Take Home Points – The Need to Know!
- Melatonin is a hormone, not a sleeping medication. It does not work for everyone.
- Melatonin tells your body it’s bedtime. It will not prevent you from waking during the night and it will not help you fall back asleep.
- Stick to physiologic dosing. 0.3 – 1mg several hours before bedtime is best in initiating sleep because it encourages your body’s own production of melatonin. Physiologic doses vary by age.
- Stay away from high dosages! Dosages of 10-50mg have been used in numerous cancer studies. Also, high amounts of melatonin have known to disrupt hormones like estrogen, progesterone, and testosterone.
- Yes, it’s used in adjunctive cancer care– but by professionals who know what they’re doing!
- Purchase physician-only brands – You’re more likely to have consistency in dosage and ingredients.
- Talk to a doctor who is knowledgeable about herbs and supplements. (Hint: it’s us, your neighborhood Naturopathic Doctor!)
References:
- Axelrod, J Shein HM, Wurtman RJ. Stimulation of C14-melatonin synthesis from C14-tryptophan by noradrenaline in rat pineal in organ culture. Proc Natl Acad Sci USA. 1969;62(2):544.
- Bruni O, Alonso-Alconada D, Besag F, Biran V, Braam W, Cortese S, Moavero R, Parisi P, Smits M, Van der Heijden K, Curatolo P. Current role of melatonin in pediatric neurology: clinical recommendations. Eur J Paediatr Neurol. 2015 Mar;19(2):122-33. Epub 2014 Dec 17.
- Di Bella, G, Mascia, F, Gualano, L, Di Bella, L; Melatonin Anticancer Effects: Review. Int. J. Mol. Sci. 2013, 14, 2410-2430.
- Di Bella G. Complete objective response to biological therapy of plurifocal breast carcinoma. Neuro. Endocrinol. Lett. 2008;29:857–866.
- Di Bella G. The Di Bella Method (DBM) improved survival, objective response and performance status in a retrospective observational clinical study on 122 cases of breast cancer. Neuro Endocrinol. Lett. 2011;32:751–762.
- Di Bella G., Biagio C. The Di Bella Method (DBM) improved survival, objective response and performance status in a retrospective observational clinical study on 23 tumors of the head and neck. Neuro Endocrinol Lett. 2012;33:249–256.
- Di Bella L. Presented at First National Conference on Melatonin: From Research to Action; Reggio Calabria. Italy, 25 January 1997.
- Di Bella L. Cancro: Siamo Sulla Strada Giusta? Travel Factory; Roma, Italy: 1997.
- Erland LA, Saxena PK. Melatonin natural health products and supplements: presence of serotonin and signi cant variability of melatonin content. J Clin Sleep Med. 2017;13(2):275–281.
- Jung, B, Ahmad, N. Melatonin in Cancer Management: Progress and Promise. (Cancer Res 2006; 66(20): 9789-93)
- Malhotra, S., Sawhney, G., Pandhi, P.; The Therapeutic Potential of Melatonin: A review of the science. MedGenMed. 2004; 6(2): 46.
- Owens, J., Rosen, C., Mindell, J.; Medication use in the Treatment of Pediatric Insomnia: Results of a survery of community-based pediatricians. Pediatrics 2003;111:e628 –e635
- Qaseem, MD, PhD, A., Kansagara, MD, D; Forciea, MD, M; Cooke, MD, M.; Denberg, MD, PhD, T; Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125-133.
- Li, Y., Li, S., Zhou, Y., Meng, X., Zhang J-J., Xu, D-P., Li, H.; Melatonin for the prevention and treatment of cancer. Oncotarget, 2017, Vol. 8, (No. 24), pp: 39896-39921.
- Luboshitzky, R., Shen-Orr, Z., Nave, R., Lavi, S., Lavie, P. Melatonin Administration Alters Semen Quality in Healthy Men. Journal of Andrology, Vol 23, No. 4. July/August 2002. pp: 572-578.
- Shamseddeen, W., Clarke, G., Keller, M., Dineen Wagner, K. Birmaher, B. Emslie, G., Ryan, N., Rosenbaum Asarnow, J., Porta, G., Brent, D. Adjunctive Sleep Medications and Depression Outcome in the treatment of serotonin-selective reuptake inhibitor resistant depression in adolescents study. J. Child and Adol Psychopharm. Vol. 22 (1). 2012. pp: 29-36.
- van Geijlswijk IM; Korzilius HPLM; Smits MG. The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. SLEEP 2010;33(12):1605-1614.
- Vural, EM, van Munster, BC. De Rooij SE. Optimal dosages for melatonin supplementation therapy in older adults: a systematic review of current literature. Drugs Aging. 2014 Jun;31(6):441-51. doi: 10.1007/s40266-014-0178-0.
- Wurtman, R. Physiology and available preparations of melatonin. Up To Date. 30 January 2019.
- Zhdanova, I, Wurtman, R, Regan, M, Taylor, J, Ping Shi, J, U. Leclair, O; Melatonin Treatment for Age-Related Insomnia, The Journal of Clinical Endocrinology & Metabolism, Volume 86, Issue 10, 1 October 2001, Pages 4727–4730
Richards M.A., Stockton D., Babb P., Coleman M.P. How many deaths have been avoided through improvements in cancer survival? BMJ. 2000;320:895–898.